UNMC mHealth Hub
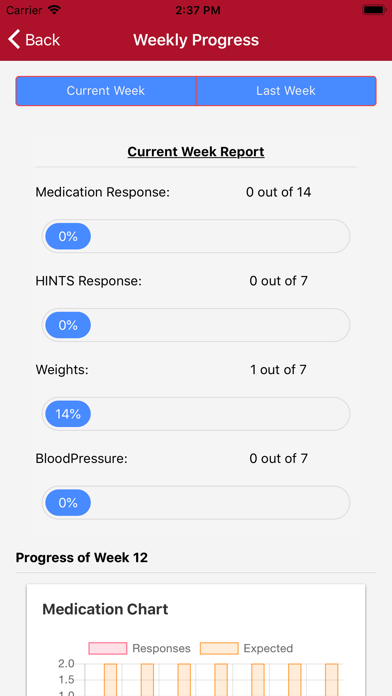
The purpose of this research is to promote individual self-management to improve adherence to treatment regimens for patients with multimorbidity. We combine evidence-based strategies used in care transition programs with a Nurse Practitioner/Community Health Worker (NP/CHW) team and mobile health (m-Health) for access and conferencing to improve adherence and other patient outcomes. To address the challenge of adherence, we use an 8 week self-management intervention with tailored self-management strategies (problem solving, decision-making, action planning, self-tailoring, resource utilization and forming a patient provider partnership), m-Health for daily messages, self-monitoring activities, and real time virtual visits. The underlying mechanisms of the interventions are to engage patients with at least two chronic diseases in self-management behaviors and treatment adherence recommendations by promoting knowledge, self-efficacy, self-management skills, and patient activation. Patients must be diagnosed with heart failure, COPD, diabetes or hypertension and at least one other chronic disease to participate in the study. The NP provides planning and follow-up care while the CHW addresses barriers to self-management. We will randomly assign 75 patients (25/group) to either Standard Care, m-Health, or m-Health Plus (receives virtual visits with NP/CHW team), using a randomized controlled trial (RCT) design with repeated measures at baseline, 1, 2 and 3 months. Specifically, we will evaluate the feasibility of the m-Health interventions, the impact of delivering each m-Health intervention compared to Standard Care, and evaluate the components of the m-health interventions. Additionally, we will test the additive impact of the NP/CHW team with the m-health technology platform.